Psoriasis: symptoms, causes, treatment & care

Psoriasis in plain language: how to recognize it and what helps
Psoriasis is a non-infectious, chronic inflammatory skin disease. It flares and remits. You can manage it by combining proper skincare, trigger control, and evidence-based therapies.
What it is
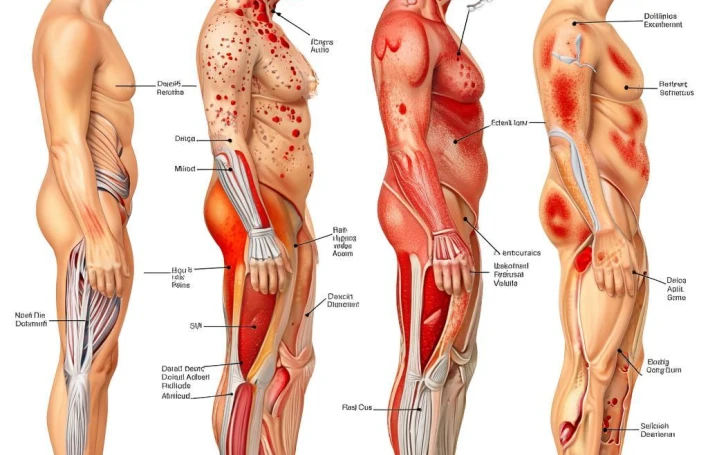
In psoriasis, the skin cell turnover speeds up, forming characteristic plaques. The disease is not contagious. It’s a systemic condition: itch, pain, nail changes, and joint involvement (psoriatic arthritis) may occur.
Symptoms
- Red plaques covered with silvery-white scales;
- Itch, tightness, fissures, sometimes pain;
- Nail changes: pitting, thickening, crumbling, onycholysis.
- Common sites: elbows, knees, scalp, lower back — but also folds (inverse psoriasis), palms/soles, etc.
Main types
- Plaque — most common (classic plaques).
- Guttate — numerous small lesions, often after a throat infection.
- Inverse — smooth lesions in skin folds (axillae, groin).
- Pustular — with pustules; requires prompt in-person assessment.
- Erythrodermic — rare but dangerous: most of the skin is involved; needs urgent care.
Triggers of flares
Stress, infections (especially streptococcal), skin trauma (Koebner phenomenon), cold/dry air, smoking, alcohol, certain meds, obesity/metabolic issues. Triggers vary by person.
When to see a doctor urgently
- Rapid spread of lesions, fever, chills;
- Signs of erythrodermic or pustular forms;
- Severe skin pain, purulent crusts;
- Joint pain/swelling, morning stiffness (possible arthritis);
- Any notable worsening in a child.
Diagnosis
Usually clinical (exam + dermoscopy). When indicated: scraping/biopsy, labs to rule out infections/metabolic problems. Photo-tracking helps monitor response to therapy.
Treatment: stepwise
- Topicals: keratolytics (salicylic acid/urea), topical corticosteroids, vitamin D analogs, calcineurin inhibitors (area/duration per physician).
- Phototherapy: narrowband UVB-311 nm — proven and safe for many forms.
- Systemic therapy: when indicated and monitored — methotrexate, cyclosporine, retinoids, targeted/biologic agents.
- Comorbidity care: weight, sleep, stress management, treating infection foci.
Home care that works
- Daily emollients (cream/ointment), especially right after showering.
- Gentle, fragrance-free cleansers; lukewarm water (5–7 minutes).
- Humidifier during the heating season.
- Avoid harsh scrubs/peels during flares.
- Sun protection (SPF) on exposed areas year-round.
FAQ
- Is psoriasis curable?
Not permanently, but modern therapies achieve long remissions and clear/almost clear skin. - How is psoriasis different from eczema?
Psoriasis tends to form thick plaques with “shiny” scales on elbows/knees/scalp; eczema more often oozes, itches intensely, and favors flexural areas. A doctor will differentiate. - Are steroid creams dangerous?
With correct potency, site, and duration they’re safe and effective. Follow the prescribed regimen and use emollients. - Does diet help?
No single “psoriasis diet.” Weight reduction (if needed), moderating alcohol, quitting smoking, and balanced nutrition often reduce flare frequency.
If you notice new plaques, significant itch or pain, or nail/joint changes, book a dermatology visit. Early adjustment of therapy typically improves quality of life and reduces flares.